|
||
      |
Eyes on melanin
As a retinal surgeon on Chicago’s South Side, Kourous Rezaei is reminded every day of an unusual health disparity. Most of his patients are African American, but nearly all his patients with a common disease, age-related macular degeneration, are Caucasian.
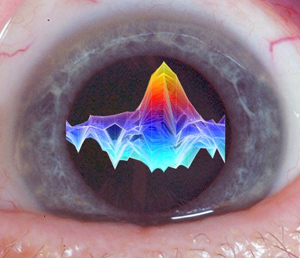
An EPR spectrum, superimposed on a photo of an eye.
Macular degeneration, the leading cause of blindness in people over age 60, triggers gradual loss of central vision. It damages RPEs—retinal pigment epithelial cells—which lie underneath the macula, the part of the retina responsible for fine detail at the field of vision’s center. Without RPE cells, the photoreceptors, or light detectors in the eye, also die. Patients lose the ability to see detail. Soon they can’t read.
It’s a “devastating disease,” says Rezaei, director of the University’s vitreoretinal service. “Imagine,” he says. “You get older, you retire, you finally have time to read—and you can’t.” Worse yet, “we do not have a cure.” Doctors can only treat the secondary complications—uncontrolled growth of blood vessels in the retina. “Since we don’t know how to replace or repair the dead or damaged retinal cells,” he says, “we need to find ways to protect them.”
Because humans stop producing RPE cells after birth, they have to last a lifetime. But they live in a hostile environment. Light constantly bombards the retina, and oxygen concentrations at the back of the eye are very high. The combination of plentiful oxygen and abundant light, especially high-energy blue light, tends to produce oxygen-free radicals—harmful substances that can damage cell membranes and DNA.
Yet macular degeneration rarely strikes African Americans. What is it, Rezaei wondered, that protects blacks from the blues? One obvious candidate was melanin, the pigment that makes dark skin dark. Melanin is found not only in the skin but throughout the body, including in the retinal cells. Scientists had long suspected that melanin could protect against light-induced damage, but evidence had shown that the pigment generated its own free radicals—the very substances researchers were trying to control.
To get a better look at melanin’s role, Rezaei began with a crucial research tool, a laboratory full of RPE cells growing in culture. Using these, he could measure melanin levels and see that cells with higher melanin content were better able to resist damage from intense blue light. But he could not prove that it was the melanin that made the difference.
So he began looking for other scientists with different tools. A long search took him a short distance—across campus—to the lab of photochemist James Norris, professor in the Department of Chemistry and the Institute for Biophysical Dynamics. Norris studies photosynthesis, in which energy from sunlight is converted into electrochemical energy—a process with many parallels to vision. To chart the early steps of photosynthesis, Norris uses electron paramagnetic resonance (EPR). EPR is similar to magnetic resonance imaging except that it measures the spin of electrons rather than of protons.
Photochemical reactions happen extremely fast, and the Norris lab has
one of the world’s few high-speed EPR spectroscopy devices, able
to record actions in nanoseconds, about 1,000 times faster than standard
EPR. “Free radicals are dangerous chemicals, and dangerous chemistry
takes place rapidly,” says Norris. “This lets us see some
of it.”
Norris had one more valuable asset: an ambitious student interested in
both chemistry and medicine, experienced with EPR, and looking for a project.
It was a unique opportunity for Brandon-Luke Seagle, a third-year student
in the College with MD/PhD aspirations.
Combining Rezaei’s cells, Norris’s technology, and Seagle’s legwork, the team captured dramatic, convincing evidence that melanin does in fact protect retinal cells. In the June 21 Proceedings of the National Academy of Sciences, they show that increased melanin aggregation and radical migration within those aggregates can protect RPE cells from free-radical damage and help prevent cell death. In the August 17 Journal of the American Chemical Society, they demonstrate how melanin actually scavenges the harmful free radicals produced by high-energy blue or ultraviolet light as it flows into the eye, soaking them up and neutralizing their effects.
“We now have the first persuasive evidence that melanin plays an important protective role within the eye,” says Norris. “Although melanin contains its own intrinsic free radical, we found that it absorbs a far more damaging form of free radical, converting its destructive energy into harmless heat before it can hurt the retina.”
The discovery has driven Rezaei back to the lab with renewed energy. “We now have molecular-based evidence to support the epidemiologic data that points to the protective effects for melanin,” he says. The next step is to begin testing ways to boost melanin levels, first in cells grown in culture and, if that experiment appears promising, in animal models.